Abstract

Introduction: Allogeneic stem cell transplantation (allo-SCT) is the best post-remission treatment for patients (pts) with acute myeloid leukemia (AML) harboring high-risk genetic features. AML with translocation t(6;9)(p23;q34) (t(6;9) AML) is a rare but well-characterized AML subtype, commonly associated to FLT3 internal tandem duplication (FLT3 -ITD). It constitutes a high-risk cytogenetic entity, with a reported high relapse risk after conventional chemotherapy. Therefore, allo-SCT in first complete remission (CR1) is now commonly recommended in these pts. However, comprehensive studies analyzing the outcome of allo-SCT in this setting are lacking.
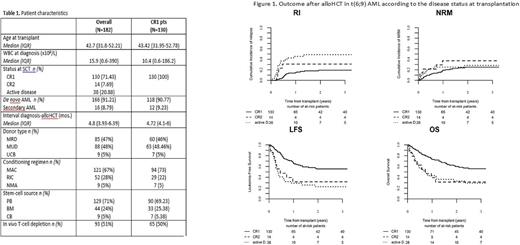
Patients and methods: We included 182 adult pts with t(6;9) AML who received an allo-SCT from 2000 to 2015, from matched related (MRD), unrelated (MUD), or cord blood donors. Statistical analyses were performed using R v3.0.1 and SPSS v19. Endpoints included leukemia-free survival (LFS), relapse incidence (RI), non-relapse mortality (NRM), overall survival (OS), acute and chronic GVHD, and GVHD-free/relapse-free survival (GRFS). All outcomes were measured from the time of stem cell infusion.
Results: Median age was 42 years (18-65 years) and 51% were male. 166 out of 182 pts (91%) presented as de novo AML. An associated cytogenetic abnormality was documented in 20 pts (11%). Among 63 (34%) pts with available information on FLT3 status, 39 (62%) carried a FLT3-ITD mutation. Status at allo-SCT was first CR (CR1) in 130 pts (71%), CR2 in 14 (8%), and non-CR AML in 38 pts (21%), respectively. The type of conditioning regimen was myeloablative in 121 (66%) of the pts. In most pts (n=129, 71%) graft source was peripheral blood. The donor was a MRD in 85 (47%), MUD in 88 (48%) and an unrelated cord blood in 9 (5%) of the pts, respectively (Table 1). With a median follow-up of 28 months, 2-year LFS was 46.7% (95% CI:38.6-54.8), OS 51.9 % (43.7-60.1), RI 26.4% (19.7- 33.6), NRM 26.9 % (20-34.2) and GRFS 33.7% (25.8-41.6). Acute GvHD grade II-IV and 2-year chronic GvHD were 26.3 % (19.9 - 33.1) and 35.7 % (27.8 - 43.6), respectively. In the univariate analysis, disease status at time of allo-SCT was the most important prognostic factor, with the following 2-year outcomes in CR1, CR2, and non-CR: RI of 19.3% (12.3-27.5), 31% (8.6-57.1) and 48.8% (31-64.4, p<0.001); LFS of 55.6% (45.8-65.3), 31.7% (6.3-57.2) and 22.7% (8.5-36.9, p<0.001); OS of 60% (50.2-69.8), 31.4% (6.1-56.8)], and 33.1% (17-49.2, p<0.001); and GRFS of 40.2% (30.2-50.1), 23.8% (0.4-47.2) and 17.2% (4.4-30.1, p<0.001), respectively (Figure 1). Reduced intensity conditioning (RIC) was associated with an increased risk of RI, without impact on LFS or OS. Secondary leukemia was associated with a reduced LFS. A longer interval (i.e., >median value, 4.8 mos.) from diagnosis to allo-SCT was associated with higher NRM. Finally, FLT3 -ITD status and additional cytogenetic abnormalities did not influence prognosis.
In pts in CR1, the main causes of death were NRM (infection, n=15; GVHD, n=9), whereas recurrent of the leukemia was the cause of death in only 12 pts. Of note, pts harboring FLT3 -ITD had a relatively favorable outcome, with a 2-year RI, NRM, LFS, OS, and GRFS of 17.2% (3.7-39.1), 27.7% (8.9-50.5), 55.1% (30.8-79.5), 57.5% (32.1-82.8), and 42.9% (19.2-66.5), respectively. In the multivariate analysis for pts in CR1, RIC was the only significant prognostic factor for RI (HR=5.79, 1.82-18.40; p=0.00293), without impact on LFS or OS.
Conclusions: Allo-SCT in patients with t(6;9) AML results in a relatively favorable outcome when performed in CR1, with approximately 17% relapse rate, suggesting the existence of a beneficial GvL effect in this context. Notably FLT3 -ITD did not show a negative impact in this entity. This study supports the recommendation to subject pts with t(6;9) AML to allo-SCT while being in CR and emphasize that allo-SCT in CR as the best current therapeutic option for these pts.
Socié: Alexion Pharmaceuticals, Inc.: Consultancy. Mohty: Sanofi: Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal